Abstract
Objective
In literature, a great diversity of limited sampling strategies (LSS) have been recommended for tacrolimus monitoring, however proper validation of these strategies to accurately predict the area under the time concentration curve (AUC0–12) is limited. The aim of this study was to determine whether these LSS might be useful for AUC prediction of other patient populations.
Methods
The LSS from literature studied were based on regression equations or on Bayesian fitting using MWPHARM 3.50 (Mediware, Groningen, the Netherlands). The performance was evaluated on 24 of these LSS in our population of 37 renal transplant patients with known AUCs. The results were also compared with the predictability of the regression equation based on the trough concentrations C0 and C12 of these 37 patients. Criterion was an absolute prediction error (APE) that differed less than 15% from the complete AUC0–12 calculated by the trapezoidal rule.
Results
Thirteen of the 18 (72%) LSS based on regression analysis were capable of predicting at least 90% of the 37 individual AUC0–12 within an APE of 15%. Additionally, all but three LSS examined gave a better prediction of the complete AUC0–12 in comparison with the trough concentrations C0 or C12 (mean 62%). All six LSS based on Bayesian fitting predicted <90% of the 37 complete AUC0–12 correctly (mean 67%).
Conclusions
The present study indicated that implementation of LSS based on regression analysis could produce satisfactory predictions although careful evaluation is necessary.
Similar content being viewed by others
Introduction
The calcineurin-inhibitor tacrolimus, used widely after organ transplantation, has a narrow therapeutic index and highly variable pharmacokinetic characteristics. Close monitoring of the drug concentration is required to achieve an optimum efficiency by minimizing the risk of subtherapeutic and toxic blood concentrations. Efficacy and side effects of tacrolimus are highly correlated with the area under the time concentration curve (AUC0–12) [1]. Elevated tacrolimus concentrations may lead to severe side effects such as nephrotoxicity, neurotoxicity and hyperglycaemia [2–4], while subtherapeutic tacrolimus concentrations increase the risk of transplant rejection enormously [5–7].
The most exact way to monitor the total tacrolimus exposure is by creating 12-h pharmacokinetic profiles, which implies that the tacrolimus concentration should be measured at at least six different time points. The AUC0–12 can then be calculated according to the trapezoidal rule using the tacrolimus concentrations measured at different time points. Since recording a complete 12-h pharmacokinetic profile for every patient is not feasible in clinical practice, traditionally many transplant centres have used tacrolimus trough (C0) concentrations to estimate the tacrolimus exposure. Although tacrolimus C0 concentrations are generally considered to be a good indication of the total systemic drug exposure [1, 8], its usefulness in differentiating graft rejection episodes from nephrotoxicity has been questioned [6, 9–11]. Recently, the correlation between individual tacrolimus concentrations and AUC0–12 has been studied in kidney [12–18], liver [19], heart [20, 21] and lung [22] transplant recipients. In these studies, a poor association was found between the tacrolimus C0 concentrations and the AUC0–12, while tacrolimus concentrations measured at other time points showed much better correlations with the AUC0–12. Additionally, strategies have been developed that included a limited number of sampling time points within a short time post-dose, the so-called limited sampling strategies (LSS). Several two- and three-time-point sampling strategies showed a high correlation with the AUC0–12 in published studies and were able to predict the AUC0–12 more accurately than the C0 concentration alone [12, 15–18, 20, 22].
Based on the number of published studies regarding LSS for tacrolimus, there seems to be a growing interest for non-C0 concentration measurements as an indicator of between-patient variability and as a guide for dose adjustments. Most of these studies recommend different LSS, but these strategies have not been validated with an independent population. Ting et al. [23] recently reported that validation of the different LSS with an independent transplant population is an absolute prerequisite. The question was whether the LSS described in literature could be used in other centres with different populations. Predictive value of LSS from literature was evaluated using our own renal post-transplant group of 37 patients with known AUCs. Also the predictive value of trough levels (C0 and C12) determined in our own population was investigated.
Materials and methods
Patient population
In total, 37 Caucasian renal transplant recipients for whom a complete 12-h time tacrolimus concentration curve had been determined in a past clinical trial were included in this study (Table 1). The transplant recipients underwent a renal transplantation at least 1 year ago. Patients taking medication known to interact with tacrolimus, who suffered from gastro-intestinal or liver disease, pre-transplantation diabetes mellitus or other disorders that could have altered the absorption of tacrolimus were excluded from this study as illustrated in Table 1.
Prior to the blood sample collection, there was no tacrolimus dose change for at least 1 week. After overnight fasting, the blood samples were collected immediately before (C0) and 0.5 (C0.5), 1 (C1), 2 (C2), 3 (C3), 4 (C4), 5 (C5), 7.5 (C7.5) and 12 (C12) h after the morning tacrolimus administration. Patients were not allowed to take food until 1 h after ingesting the tacrolimus dose and were advised to avoid grapefruit intake to prevent alterations in the tacrolimus metabolism. Demographic as well as clinical data were determined at the time of recording the 12-h time tacrolimus concentration curve. The study was performed in accordance with the Declaration of Helsinki and its amendments. The protocol was approved by the local Medical Ethics Committee and written informed consent for participation in this study was obtained from all patients.
Determination of tacrolimus concentrations
The tacrolimus blood concentrations were determined in ethylene diamine tetra-acetic acid (EDTA) whole blood, using a method based on high-pressure liquid chromatography tandem mass spectrometry (HPLC-MS/MS). The assay is linear from 1 to 300 μg/l. Intra-assay precision and accuracy were 3.4, 2.2, and 3.0% and 102, 94 and 94% respectively at 3.04, 6.23 and 13.0 μg/l (n = 6). Inter-assay precision and accuracy were 8.2, 5.2, and 4.6% and 102, 94 and 93% (n = 9) respectively. Lower limit of quantification was 1.0 μg/l. The laboratory participates in the International Tacrolimus Proficiency Testing Scheme.
Limited sampling strategies investigated
In our opinion, a suitable limited sampling strategy for tacrolimus should consist of two or three time concentration points within a short time post-dose (≤4 h) including a trough level. We selected 24 LLS from the literature [12, 15, 16, 18, 20, 22]. Eighteen of these strategies were based on regression analysis [12, 16, 18, 20, 22], and six other strategies were based on Bayesian fitting [15]. Also strategies based on the tacrolimus C0 and C12 concentrations were developed for our own renal transplant patient population and compared with above-mentioned LSS.
Pharmacokinetics and statistical analysis
The area under the tacrolimus time concentration curve (AUC0–12) was calculated from the time versus tacrolimus concentration plot using the linear trapezoidal rule in MWPharm 3.50 (Mediware, Groningen, The Netherlands). The predicted AUC0–12 (AUCpred), calculated with the 24 different LSS, were validated by determining the predictive performance as described by Sheiner and Beal [24]. The percentage of the prediction error (PE) and the percentage of the absolute prediction error (APE) are parameters often used for validation in LSS [12, 14–16, 18, 20, 22]. Given the high pharmacokinetic variability, an APE of less than 15% was considered clinically acceptable [16, 25, 26].
Prediction bias was measured as a percentage of the prediction error [PE (%)] using the following formula:
Prediction precision was measured as a percentage of the APE using the following formula:
The variance in the strength of association between the AUCpred and the AUCactual was reflected by the linear regression coefficient of multiple determination (R 2). All values are expressed as mean ± SD. All statistical analyses were performed with use of SPSS 12.0 software for windows (Chicago, IL, USA).
Results
Evaluation of predictive performances of the limited sampling strategies
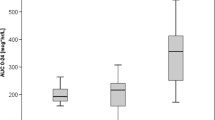
Table 2 shows an overview of the studies describing the LSS evaluated in the present study. The regression equations and the R 2 found by the investigators for the evaluated LSS are summarised in Table 3. Table 4 describes the R 2, which represents the association between AUCpred and AUCactual and the calculated PE and APE of the 24 evaluated LSS for our 37 pharmacokinetic profiles. Thirteen of the 18 LSS (72%) based on regression analysis had a predictivity of >90%. Additionally, all except three of the LSS examined gave a better prediction of the complete AUC0–12 in comparison with LSS based on a trough concentration C0 and C12 (mean 62%). Predictivity of all six LSS based on Bayesian fitting was <90% (mean 66.8%). Additionally, Fig. 1 illustrates an overview of the performances of the 26 LSS evaluated in our well-characterized population of renal transplant recipients.
An overview of the predictive performances of the limited sampling strategies published using 37 different pharmacokinetic profiles recorded in our renal transplant recipients. The number of limited sampling strategies categorized into the percentage of AUC0–12 within a prediction error of <15% is plotted on the x-axis, the number of limited sampling strategies is plotted on the y-axis
Discussion
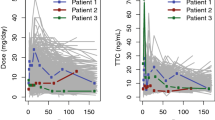
Our results confirm the results of several other studies [12, 14–16, 18, 20, 22] that trough concentrations C0 and C12 have a lower predictive value for the complete 12-h AUC than almost all other studied LSS. The predictivity of LSS based on Bayesian estimation of the AUCactual was lower than the LSS based on regression analysis. Therefore a trough level and one or two time points in the early phase (≤4 h) post-dose seem not to be sufficient for a Bayesian estimation strategy to fit correctly most of the AUC0–12 and thus predict the complete AUC0–12 reliably. The differences in variability and shape between the curves of post-transplant recipients combined with just two or three sample points might have been caused by the large differences found between the AUCpred calculated according to the Bayesian estimation strategy and the complete AUCactual.
In contrast to most studies that describe LSS for tacrolimus in literature, we used an HPLC-MS/MS assay to determine the tacrolimus concentration. Because there seems to be a fixed difference of about 15% between the immunoassay and the HPLC-MS/MS, the prediction will change proportionally, and the predictivity of the LSS will be the same. Also potential interfering drug-drug interactions will have an equal influence on the different tacrolimus concentrations, which consequently has no effect on the predictivity of the different LSS.
Ting et al. [23] recently suggested that LSS should only be applied on transplant patient populations that are comparable with the transplant patient population that was used to develop the LSS. However, the renal transplant patient group examined in the present study was not exactly comparable with the transplant patient populations in which the equations for the LSS were developed. For example Aumente Rubio et al. [20] and Ragette et al. [22] used heart and lung transplant recipients respectively to develop and validate their LSS. Despite the fact that the LSS were developed with the pharmacokinetic profiles of patients who underwent a different kind of transplantation, Eqs. (5), (24) and (26) were able to predict at least 90% of the AUC0–12 within an APE of 15%, which suggests that these LSS are more robust than expected by Ting et al. [23]. Even though LSS gave a better reflection of the tacrolimus exposure, they are currently not often applied by clinical transplant practioners, possibly for logistical and financial reasons.
In conclusion, after validating several LSS from the literature, the present study indicates that all but three LSS gave a better prediction of the complete AUC0–12 than the trough concentrations C0 or C12. Moreover, LSS could produce satisfactory predictions for AUC0–12 recorded in an independent renal transplant patient population, although further evaluation of their reliability is necessary.
References
Mahalati K, Kahan BD (2000) Pharmacological surrogates of allograft outcome. Ann Transplant 5(2):14–23
Winkler M, Christians U (1995) A risk-benefit assessment of tacrolimus in transplantation. Drug Saf 12(5):348–357
McMaster P, Mirza DF, Ismail T, Vennarecci G, Patapis P, Mayer AD (1995) Therapeutic drug monitoring of tacrolimus in clinical transplantation. Ther Drug Monit 17(6):602–605
Staatz CE, Tett SE (2004) Clinical pharmacokinetics and pharmacodynamics of tacrolimus in solid organ transplantation. Clin Pharmacokinet 43(10):623–653
Laskow DA, Vincenti F, Neylan JF, Mendez R, Matas AJ (1996) An open-label, concentration-ranging trial of FK506 in primary kidney transplantation: a report of the United States Multicenter FK506 Kidney Transplant Group. Transplantation 62(7):900–905
Kershner RP, Fitzsimmons WE (1996) Relationship of FK506 whole blood concentrations and efficacy and toxicity after liver and kidney transplantation. Transplantation 62(7):920–926
Undre NA, van Hooff J, Christiaans M, Vanrenterghem Y, Donck J, Heeman U et al (1999) Low systemic exposure to tacrolimus correlates with acute rejection. Transplant Proc 31(1–2):296–298
Braun F, Schutz E, Peters B, Talaulicar R, Grupp C, Undre N et al (2001) Pharmacokinetics of tacrolimus primary immunosuppression in kidney transplant recipients. Transplant Proc 33(3):2127–2128
Backman L, Nicar M, Levy M, Distant D, Eisenstein C, Renard T et al (1994) Whole blood and plasma levels of FK 506 after liver transplantation: correlation with toxicity. Transplant Proc 26(3):1804
Takahara S, Kokado Y, Kameoka H, Takano Y, Jiang H, Moutabarrik A et al (1994) Monitoring of FK 506 blood levels in kidney transplant recipients. Transplant Proc 26(4):2106–2108
Winkler M, Ringe B, Rodeck B, Melter M, Stoll K, Baumann J et al (1994) The use of plasma levels for FK 506 dosing in liver-grafted patients. Transpl Int 7(5):329–333
Armendariz Y, Pou L, Cantarell C, Lopez R, Perello M, Capdevila L (2005) Evaluation of a limited sampling strategy to estimate area under the curve of tacrolimus in adult renal transplant patients. Ther Drug Monit 27(4):431–434
Balbontin FG, Kiberd B, Squires J, Singh D, Fraser A, Belitsky P et al (2003) Tacrolimus monitoring by simplified sparse sampling under the concentration time curve. Transplant Proc 35(7):2445–2448
Kuypers DR, Claes K, Evenepoel P, Maes B, Coosemans W, Pirenne J et al (2004) Time-related clinical determinants of long-term tacrolimus pharmacokinetics in combination therapy with mycophenolic acid and corticosteroids: a prospective study in one hundred de novo renal transplant recipients. Clin Pharmacokinet 43(11):741–762
Scholten EM, Cremers SC, Schoemaker RC, Rowshani AT, van Kan EJ, den Hartigh J et al (2005) AUC-guided dosing of tacrolimus prevents progressive systemic overexposure in renal transplant recipients. Kidney Int 67(6):2440–2447
Wong KM, Shek CC, Chau KF, Li CS (2000) Abbreviated tacrolimus area-under-the-curve monitoring for renal transplant recipients. Am J Kidney Dis 35(4):660–666
Stolk LM, Van Duijnhoven EM, Christiaans MH, van Hooff JP (2002) Trough levels of tacrolimus. Ther Drug Monit 24(4):573; author reply, 4
Pisitkun T, Eiam-Ong S, Chusil S, Praditpornsilpa K, Pansin P, Tungsanga K (2002) The roles of C4 and AUC0-4 in monitoring of tacrolimus in stable kidney transplant patients. Transplant Proc 34(8):3173–3175
Ku YM, Min DI (1998) An abbreviated area-under-the-curve monitoring for tacrolimus in patients with liver transplants. Ther Drug Monit 20(2):219–223
Aumente Rubio MD, Arizon del Prado JM, Lopez Malo de Molina MD, Cardenas Aranzana M, Segura Saint-Gerons J, Lopez Granados A et al (2003) Clinical pharmacokinetics of tacrolimus in heart transplantation: new strategies of monitoring. Transplant Proc 35(5):1988–1991
Sgrosso JL, Araujo GL, Vazquez MC (2002) Tacrolimus pharmacokinetics in heart transplant. Transplant Proc 34(1):142–143
Ragette R, Kamler M, Weinreich G, Teschler H, Jakob H (2005) Tacrolimus pharmacokinetics in lung transplantation: new strategies for monitoring. J Heart Lung Transplant 24(9):1315–1319
Ting LS, Villeneuve E, Ensom MH (2006) Beyond cyclosporine: a systematic review of limited sampling strategies for other immunosuppressants. Ther Drug Monit 28(3):419–430
Sheiner LB, Beal SL (1981) Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm 9(4):503–512
Meier-Kriesche HU, Kaplan B, Brannan P, Kahan BD, Portman RJ (1998) A limited sampling strategy for the estimation of eight-hour neoral areas under the curve in renal transplantation. Ther Drug Monit 20(4):401–407
David OJ, Johnston A (2001) Limited sampling strategies for estimating cyclosporin area under the concentration-time curve: review of current algorithms. Ther Drug Monit 23(2):100–114
Acknowledgements
We would like to thank Mrs Monique Mullens and Mr John Dackus (Department of Internal Medicine, University Hospital Maastricht, the Netherlands) for their excellent work regarding the extensive blood sample collection required to record a pharmacokinetic profile for each renal transplant patient.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Op den Buijsch, R.A.M., van de Plas, A., Stolk, L.M.L. et al. Evaluation of limited sampling strategies for tacrolimus. Eur J Clin Pharmacol 63, 1039–1044 (2007). https://doi.org/10.1007/s00228-007-0354-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-007-0354-9