Abstract
Background:
Although medical care for very-low-birth-weight (VLBW) infants has improved over time, it is unclear how this has affected mortality and morbidity. To characterize these trends, a network database was analyzed.
Methods:
This is a cohort study of VLBW infants born from 2003 through 2008.
Results:
Over the 6-y period, 19,344 infants were registered and analyzed. Crude mortality rates among the infants at discharge decreased significantly (from 10.8 to 8.7%) during the study period. The greatest improvement in mortality was observed among infants with birth weights between 501 and 750 g (25.6–17.7 %). The odds ratio (OR) of mortality over year adjusted for potential confounders by a logistic regression model was 0.94 (95% confidence interval 0.92–0.97). Significant increases were observed in some morbidities, including symptomatic patent ductus arteriosus with an OR of 1.11 (1.09–1.13); late-onset adrenal insufficiency, 1.21 (1.17–1.26); and necrotizing enterocolitis/intestinal perforation, 1.10 (1.01–1.12). However, the severe form of intraventricular hemorrhage, with an OR of 0.98 (0.92–0.99), decreased significantly. Risk-adjusted trends in other morbidities showed no significant change.
Conclusion:
Mortality of VLBW infants decreased significantly over the 6-y study period. Decreasing morbidity is essential for further improvement in the outcomes in VLBW infants.
Similar content being viewed by others
Main
Even though there have been continual advances in neonatal care and a decline in neonatal mortality in the past several decades, there is still significant room for improvement in morbidity and mortality among low-birth-weight infants (1,2,3,4). To establish best practices for the prevention of morbidity and mortality in low-birth-weight infants, continuous monitoring of the outcomes among high-risk infants is essential. For this purpose, a neonatal research network database created with a grant from the Ministry of Health, Labour, and Welfare of Japan has been operating since 2003 (5). The database includes infants with birth weights at or less than 1,500 g, herein referred to as very-low-birth-weight (VLBW) infants, who were treated in participating neonatal centers. Both outcomes and interventions in VLBW infants may have changed since the database was established. To characterize these trends, morbidity and mortality in infants born in 2003–2008, the first 6-y period of the database, were analyzed in this study. Furthermore, factors affecting the improved or aggravated outcomes were also analyzed. Standardization of treatment of VLBW infants through this kind of analysis could help to improve the outcomes of VLBW infants on a nation-wide basis.
Results
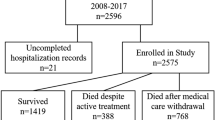
Participating Hospitals and Registered Infants
Table 1 shows annual characteristics of the participating hospitals. The number of registered infants increased as the number of participating hospitals increased, whereas the average number of infants per hospital decreased slightly. This suggests that smaller hospitals have recently started participating in the network. Considering the nation-wide population of VLBW infants born in Japan during the study period, more than 50% of VLBW infants in Japan were in the registry. Finally, the trend of gestational age distribution of the infants showed a constant ratio.
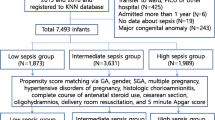
Trends in Antenatal and Neonatal Factors
Table 2 shows trends in antenatal and neonatal factors among the registered infants. Among antenatal factors, maternal age, incidence of pregnancy-induced hypertension, and antenatal steroid (ANS) use significantly increased during the study period. On the other hand, ratios of primipara, head presentation, outborn infants, and Apgar scores <4 at 1 min decreased. Gestational age and birth weight of the infants remained constant, which again indicates the uniformity of the database. The incidence of diabetic mothers, clinical chorioamnionitis, prolonged rupture of membranes, and fetal heart rate abnormalities (nonreassuring of fetal status) did not change significantly during the study period. The ratio of cesarean sections and the incidence of major congenital anomalies also did not show any significant trend.
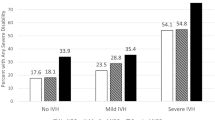
Trends in Morbidity, Interventions, and Mortality
Table 3 shows trends in morbidity, interventions, and mortality among the registered infants. The rate of infants who were deceased at discharge significantly decreased over time. However, respiratory distress syndrome, symptomatic patent ductus arteriosus (PDA), late-onset adrenal insufficiency of prematurity, and necrotizing enterocolitis (NEC) and/or intestinal perforation increased significantly. On the other hand, the incidence of grade III and IV intraventricular hemorrhages (IVHs) decreased significantly. Among interventions, endotracheal intubation for resuscitation at birth, inhaled nitric oxide, indomethacin or surgical ligation for PDA, intravenous hyperalimentation, and laser photocoagulation for retinopathy of prematurity increased significantly. Other morbidities and interventions remained unchanged during the study period.
Adjusted Trends in Morbidity, Interventions, and Mortality
A multivariable logistic model with deceased at discharge as the dependent variable and the potential risk factors described above as the independent variable was analyzed. As a result, multiple pregnancies with an odds ratio (OR) of 1.17 (confidence interval (CI) 1.03–1.33); pregnancy-induced hypertension, OR 0.70 (CI 0.59–0.83); ANS, OR 0.62 (CI 0.55–0.69); nonreassuring of fetal status, OR 1.34 (CI 1.20–1.50); presentation of the fetus (head), OR 0.87 (CI 0.77–0.97); mode of delivery (cesarean section), OR 0.78 (CI 0.69–0.87); gestational age >37 or <24 wk, OR 2.20 (CI 1.93–2.50); birth weight (100 g), OR 0.74 (CI 0.72–0.76); male gender, OR 1.30 (CI 1.17–1.44); Apgar score <4 at 1 min, OR 2.82 (CI 2.53–3.14); and major congenital anomalies, OR 13.88 (CI 11.95–16.11) were considered independent variables associated with being deceased at discharge in this data set. These factors were used to adjust for changes in background risks over time. Furthermore, the 39 hospitals that had participated in the network database for the entire study period were chosen. These original 39 hospitals contributed 12,863 infants to the database. The logistic model was applied to those infants with adjusted risk factors. Table 4 shows the factors that changed significantly over time. Deceased at discharge decreased significantly over the whole study period, and as a single-year change for each year except 2005.
Similarly, morbidities such as symptomatic PDA, late-onset adrenal insufficiency of prematurity, severe IVH, and NEC and/or intestinal perforation significantly changed during the study period according to the logistic model. Interventions that increased significantly over the study period included inhaled nitric oxide, indomethacin for PDA, PDA ligation, intravenous hyperalimentation, and retinopathy of prematurity treatment. Figure 1 shows the trends in mortality, morbidity, and interventions that showed significant trend changes with the logistic model among the 39 hospitals. These trends were equally significant among all of the participating hospitals using the same logistic model.
Trends in mortality, morbidity, and interventions among the 39 hospitals. Number of infants analyzed was 12,863. (a) Deceased at discharge (filled squares). (b) Indomethacin for PDA, PDA ligation, and symptomatic PDA. Filled squares, indomethacin for PDA; filled triangles, PDA ligation; filled diamonds, symptomatic PDA. (c) IVH grade III or IV, NEC and/or intestinal perforation, and late-onset AOP. Filled squares, IVH III or IV; filled triangles, NEC and/or intestinal perforation; filled diamonds, late-onset AOP. (d) Intravenous hyperalimentation, ROP treatment, and iNO. Filled squares, intravenous hyperalimentation; filled triangles, ROP treatment; filled diamonds, iNO. AOP, adrenal insufficiency of prematurity; iNO, inhaled nitric oxide; IVH, intraventricular hemorrhage; NEC, necrotizing enterocolitis; PDA, patent ductus arteriosus; ROP, retinopathy of prematurity.
Trends in Mortality by Birth Weight and Gestational Age
Figure 2 shows trends in mortality among different birth weight and gestational age categories. The P value by the Cochrane–Armitage χ2 test for each birth weight and gestational age category was lowest among infants with birth weights between 501 and 750 g (P = 0.03).
Trends in mortality by birth weight and gestational age. (a) Mortality by birth weight. Filled squares, −500 g (P = 0.31); filled triangles, 501–750 g (P = 0.03)*; filled diamonds, 751–1,000 g (P = 0.05); black crosses, 1,001–1,250 g (P = 0.71); filled circles, 1,251–1,500 g (P = 0.44). P values were calculated by the Cochrane–Armitage χ2 test. *Significant decrease. (b) Mortality by gestational age. Filled squares, 22–24 wk (P = 0.05)**; filled triangles, 25–27 wk (P = 0.21); filled diamonds, 28–30 wk (P = 0.93); black crosses, 31–33 wk (P = 0.06); filled circles, 34 wk- (P = 0.42). P values were calculated by the Cochrane–Armitage χ2 test. **Significant decrease.
Discussion
The most important trend over the 6-y study period is the significant decrease in the mortality rate. This decreased mortality was consistent among the single infants at an OR of 0.96 (CI 0.92–0.99). Furthermore, the most significant improvement was observed among infants with birth weights between 501 and 750 g or with a gestational age between 22 and 24 wk. As shown in Table 1 , the proportion of infants registered with this gestational age remained constant, indicating a constant attitude of resuscitation toward infants with a marginal viability. Therefore, it was unlikely that the selection bias of the infants with marginal viability occurred during the study period.
The survival rate dramatically increased in infants with a gestational age between 22–24 and 25–27 wk and a birth weight >500 g. On the other hand, the survival rate among the infants with a gestational age of more than 28 wk or a birth weight >750 g was already sufficiently low. Only exceptionally critical infants with complications such as congenital anomalies would not survive. Thus, for further improvement of survival rates in VLBW infants, there would be no other option besides improvement among infants at the threshold of variability, including infants with a birth weight of <500 g or a gestational age between 22 and 24 wk. If viability is defined by a survival rate of equal to or >50%, these infants already meet these criteria. However, the definition does not take into account the long-term outcomes. To pursue improvement in short- and long-term outcomes, extraordinary efforts greater than before and a public agreement to intervene in the cases of these critically ill infants will be mandatory.
An important difference in prenatal care over the study period was the increased rate of ANS. Because ANS was previously used off-label in Japan, the average use of ANS in VLBW infants was around 40% at the time this database was established. Since then, the use of ANS has gradually increased. In 2009, maternal steroids were finally labeled for use by the national government. Because ANS was actually a risk factor for mortality in the present logistic model, the increased use of ANS may partially explain the improved outcomes in VLBW infants. Even though ANS is reported to have advantages even for infants born at <24 gestational wk (6), the logistic model adjusted without ANS indicated that only 15% of the reduced mortality could be attributed to the increase in ANS. On the other hand, although being delivered by cesarean section was an independent risk factor for mortality in the logistic model, the rate of cesarean delivery did not change significantly during the study period. Therefore, the improved mortality among the infants was not correlated with cesarean sections. Both the incidence of symptomatic PDA and the use of indomethacin increased significantly during the study period. These increases were assumed to have been derived from early diagnosis and interventions for PDA, not by an actual increase of PDA. Furthermore, prophylactic use of indomethacin was also accepted by the participating hospitals (7,8,9). Regardless of the increased use of indomethacin, the rate of PDA ligation has not decreased. This result might indicate that the incidence of severe PDA, which could be treated only by surgical ligation at birth, was independent of medical interventions after birth. On the other hand, severe IVH may be responsible for poor neurological outcomes as opposed to mortality. This study clearly showed a decreased incidence of severe IVH, suggesting improved developmental outcomes among the survivors. Although it is not clear which interventions might contribute to the decreased incidence of severe IVH, in this condition, the increased use of indomethacin could be one contributor. Although ANS was reported to reduce the risk of IVH in VLBW infants, in this study the decreased incidence of severe IVH was significant even after adjustment for the use of ANS (10).
Late-onset adrenal insufficiency of prematurity, which is defined as glucocorticoid use during the hospital stay for treatment of late-onset circulatory collapse of premature infants due to impaired adrenal function, seems to be continually increasing. Even though this morbidity is not correlated with mortality directly, it correlates strongly with poor neurological outcomes (11). Early diagnosis seems to be important for this condition (12). Increased incidence of NEC and/or intestinal perforation is another issue. The incidence of NEC remained low in this study population. However, efforts to analyze the background risk factors for the onset of NEC and efforts to find a way to decrease this morbidity are ongoing.
One reason for the increase in the use of intravenous hyperalimentation and inhaled nitric oxide for preterm infants could be simply the dissemination of experience. Many facilities are now familiar with these interventions and are using them effectively and safely. An explanation for the increased rate of retinopathy of prematurity treatment was difficult to formulate because the decision for such treatment was totally dependent on the decision of the ophthalmologists (13).
In some cases it is not accurate to compare the outcomes of high-risk infants among different databases directly, because the background characteristics of the infants registered may not be same. If the outcomes of the present data were compared with other large databases for the same birth year, the mortality rate in Japanese neonatal intensive care units would be relatively low (14,15,16,17,18). To make an interdatabase comparison possible, an organization for internal collaborative study must be created.
There were limitations to this study. Even though the proportion of VLBW infants registered in the database exceeded 50% nationally and the number of participating hospitals increased over time, almost half of the VLBW infants were delivered and treated outside the network database. The effort to involve all hospitals in the network database must be continued. Another limitation of the study was the lack of analysis of long-term outcomes. Analyses with a primary outcome of intact survival will answer questions concerning best practices for VLBW infants.
According to the database analysis, improved mortality over the 6 y of this study among VLBW infants was clear. Further analysis of the relationship between individual interventions and outcome measures is important for understanding and improving the care of the VLBW infant. For this purpose, the nation-wide database currently in use is important and must be continued.
Methods
Patient Selection
All VLBW infants who were born in or transferred within 28 d of birth to participating neonatal centers between January 2003 and December 2008 were included in the study. VLBW infants who were born alive but died in the delivery room were also registered. A total of 82 level III perinatal centers were registered in the database and are listed in the Appendix.
Definitions
To define patient characteristics, 119 characteristics of each infant were recorded retrospectively until discharge in accordance with the network database operation manual. In the manual, the date of birth was defined as “day 0.” Mortality was defined as death occurring before discharge from a participating neonatal intensive care unit. Gestational age was expressed as completed age as determined by obstetric examination with ultrasonography early during the pregnancy or, if an early ultrasound was unavailable, via obstetric history based on the last menstrual period. All other factors were defined as has been previously reported (5).
Included in this study were VLBW infants who were born alive but died in the delivery room (delivery room resuscitation failure), which remained almost constant at <1% of the total number of infants registered each year. The network defines stillbirth as an infant who did not show any cardiac pulse under vigorous resuscitation after 22 wk of gestational age regardless of birth weight. However, the number of stillbirths was not collected in the network database. Therefore, the denominator of the database was the number of the infants born alive in the participating hospitals and infants transferred to the participating hospitals within 28 d after birth.
Statistics
One-way ANOVA or the Kruskal–Wallis test was used to test the difference over time for numerical variables where appropriate. The χ2 test for trends in proportions (Cochran–Armitage test) was used to test the change over time for categorical data.
Because the number of hospitals participating in the registry increased each year and the clinical condition of the infants admitted among hospitals may not be constant, trends over time of mortality and morbidity were examined while controlling for background risk factors. To assess trends over time, year was included as either a continuous or binary dummy variable with background risks adjusted. A multivariable logistic regression analysis with mortality as the dependent variable was first performed to determine perinatal risk factors for mortality. These risk factors included maternal age, number of deliveries, multiple pregnancies, maternal diabetes, pregnancy-induced hypertension, chorioamnionitis, prolonged rupture of membranes, ANS, nonreassuring of fetal status, delivery presentation, mode of delivery, gestational age, birth weight, gender, place of birth, Apgar score at 1 min, and associated major congenital anomalies, which were determined based on clinical relevance. A gestational age of >37 or <24 wk was used as a risk factor for deceased at discharge, according to the cumulative data in our network database (http://plaza.umin.ac.jp/nrndata/reports/nrn4_all.pdf). The mortality rate exceeded 30% among the infants with this risk factor. Independent variables identified with this logistic model were further used to analyze trends over time.
To analyze trends in morbidity, interventions, and mortality among the infants during the study period, another multiple logistic regression model was established. In this model, all variables that were independent risk factors for mortality were mandatorily included. The absence of multicollinearity among these variables was confirmed with a correlation coefficient matrix in advance. To avoid bias among participating hospitals, 39 hospitals were chosen for the second logistic model because they were continuously tracked in the database during the entire 2003–2008 study period.
All statistical analyses were performed using the SPSS, version 14.0J (IBM SPSS Japan, Tokyo, Japan). Differences were considered statistically significant at P < 0.05. However, only variables with P < 0.01 at univariate analysis were entered into the multivariable model as covariates, because the data set was very large, and too many variables reduce the performance of multiple analyses.
All information about the infants was collected anonymously, and the stored data were unlinked from individual data. The protocol of this study was approved by the central internal review board at Tokyo Women’s Medical University, where all data were collected and stored.
Appendix
List of Institutions and Representative Physicians Enrolled in the Database for Neonatal Research Network, Japan
Sapporo City General Hospital: S. Hattori; Kushiro Red Cross Hospital: A. Noro; Aomori Prefectural Central Hospital: T. Amizuka; Iwate Medical University: S. Chida; Sendai Red Cross Hospital: R. Takahashi; Akita Red Cross Hospital: H. Arai; Fukushima Medical University: T. Imamura; National Fukushima Hospital: N. Ujiie; University of Tsukuba: Y. Miyazono; Tsuchiura Kyodo General Hospital: J. Shimizu; Dokkyo Medical University: H. Suzumura; Jichi Medical University: Y. Kono; Saitama Children’s Medical Center: M. Shimizu; Saitama Medical University Saitama Medical Center: T. Kunikata; Gunma Children’s Medical Center: T. Fujiu; Kameda Medical Center: H. Sato; Tokyo Women’s Medical University Yachiyo Medical Center: T. Kondo; Tokyo Metropolitan Bokuto Hospital: T. Watanabe; Showa University: M. Aizawa; Tokyo Women’s Medical University: A. Uchiyama; Nihon University Itabashi Hospital: M. Makimoto; Teikyo University: J. Hoshi; Toho University: H. Yoda; Japan Red Cross Medical Center: Y. Kawakami; Aiiku Hospital: N. Ishii; National Center for Child Health and Development: Y. Ito; Kanagawa Children’s Medical Center: H. Itani; Yokohama City University Medical Center: K. Seki; Tokai University: M. Nomura; Kitazato University: M. Nowatari; Yamanashi Prefectural Central Hospital: A. Nemoto; Nagaoka Red Cross Hospital: O. Nagata; Niigata City Hospital: Y. Nagayama; Nagano Children’s Hospital: T. Nakamura; Shinshu University: M. Okada; Iida City Hospital: S. Nakata; National Nagano Hospital: E. Shimazaki; Saku General Hospital: T. Yoda; Toyama Prefectural Central Hospital: T. Hutatani; Ishikawa Prefectural Central Hospital: Y. Ueno; Fukui Prefectural Hospital: K. Iwai; Shizuoka Children’s Hospital: Y. Nakazawa; Seirei Hamamatsu General Hospital: S. Oki; Nagoya Red Cross First Hospital: C. Suzuki; National Mie Hospital: M. Bonno; Gifu Prefectural Central Hospital: Y. Kawano; Otsu Red Cross Hospital: K. Nakamura; Kyoto Red Cross First Hospital: N. Mitsufuji; Osaka Medical Center and Research Institute for Maternal and Child Health: J. Shiraishi; Osaka City General Hospital: H. Ichiba; Takatsuki Hospital: H. Minami; Yodogawa Christian Hospital: H. Wada; Kansai Medical University: A. Ohashi; Aizenbashi Hospital: K. Sumi; Nara Medical University: Y. Takahashi; Wakayama Prefectural Medical University: T. Okutani; Hyogo Prefectural Kobe Children’s Hospital: S. Yoshimoto; Tottori University: I. Nagata; Shimane Prefectural Central Hospital: E. Kato; Kurashiki Central Hospital: S. Watabe S; National Okayama Hospital: M. Kageyama; Hiroshima Prefectural Hospital: R. Fukuhara; Hiroshima City Hospital: M. Hayashitani; Yamaguchi Prefectural Medical Center: K. Hasegawa; National Kagawa Children’s Hospital: A. Ohta; Kagawa University: T. Kuboi; Ehime Prefectural Central Hospital: S. Akiyoshi; Kochi Health Sciences Center: K. Kikkawa; Tokushima University: T. Saijo; St. Mary’s Hospital: S. Shimokawa; Kitakyushu City Municipal Medical Center: N. Matsumoto; Kurume University: H. Kanda; Fukuoka University: E. Oota; National Kyushu Medical Center: G. Kanda; Kyushu University: M. Ochiai; National Nagasaki Medical Center: M. Aoki; Kumamoto City Hospital: Y. Kondo; Kumamoto University: M. Iwai; Oita Prefectural Hospital: K. Iida; Miyazaki University: T. Ikenoue; Kagoshima City Hospital: S. Ibara; Okinawa Chubu Hospital: M. Kohama.
Statement of Financial Support
This study was partly supported by a grant from the Ministry of Health, Labor and Welfare, Japan.
Disclosure
The authors declared no conflict of interest.
References
Hack M, Horbar JD, Malloy MH, Tyson JE, Wright E, Wright L . Very low birth weight outcomes of the National Institute of Child Health and Human Development Neonatal Network. Pediatrics 1991;87:587–97.
Horbar JD, Badger GJ, Carpenter JH, et al.; Members of the Vermont Oxford Network. Trends in mortality and morbidity for very low birth weight infants, 1991–1999. Pediatrics 2002;110(1 Pt 1):143–51.
Fanaroff AA, Stoll BJ, Wright LL, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol 2007;196:147.e1–8.
Itabashi K, Horiuchi T, Kusuda S, et al. Mortality rates for extremely low birth weight infants born in Japan in 2005. Pediatrics 2009;123:445–50.
Kusuda S, Fujimura M, Sakuma I, et al. Morbidity and mortality of infants with very low birth weight in Japan: center variation. Pediatrics 2006;118:e1130–8.
Mori R, Kusuda S, Fujimura M; Neonatal Research Network Japan. Antenatal corticosteroids promote survival of extremely preterm infants born at 22 to 23 weeks of gestation. J Pediatr 2011;159:110–114.e1.
Ment LR, Oh W, Ehrenkranz RA, et al. Low-dose indomethacin and prevention of intraventricular hemorrhage: a multicenter randomized trial. Pediatrics 1994;93:543–50.
Ment LR, Vohr B, Allan W, et al. Outcome of children in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics 2000;105(3 Pt 1):485–91.
Yanowitz TD, Baker RW, Sobchak Brozanski B . Prophylactic indomethacin reduces grades III and IV intraventricular hemorrhages when compared to early indomethacin treatment of a patent ductus arteriosus. J Perinatol 2003;23:317–22.
Ment LR, Oh W, Ehrenkranz RA, Philip AG, Duncan CC, Makuch RW . Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol 1995;172:795–800.
Nakanishi H, Yamanaka S, Koriyama T, et al. Clinical characterization and long-term prognosis of neurological development in preterm infants with late-onset circulatory collapse. J Perinatol 2010;30:751–6.
Masumoto K, Kusuda S, Aoyagi H, et al. Comparison of serum cortisol concentrations in preterm infants with or without late-onset circulatory collapse due to adrenal insufficiency of prematurity. Pediatr Res 2008;63:686–90.
Jones JG, MacKinnon B, Good WV, et al. The early treatment for ROP (ETROP) randomized trial: study results and nursing care adaptations. Insight 2005;30:7–13.
Kutz P, Horsch S, Kühn L, Roll C . Single-centre vs. population-based outcome data of extremely preterm infants at the limits of viability. Acta Paediatr 2009;98:1451–5.
EXPRESS Group, Fellman V, Hellström-Westas L, Norman M, et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA 2009;301:2225–33.
Stoll BJ, Hansen NI, Bell EF, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010;126:443–56.
Lee HC, Green C, Hintz SR, et al. Prediction of death for extremely premature infants in a population-based cohort. Pediatrics 2010;126:e644–50.
Shah PS, Ye XY, Synnes A, Rouvinez-Bouali N, Yee W, Lee SK . Prediction of survival without morbidity for infants born at under 33 weeks gestational age: a user-friendly graphical tool. Arch Dis Child Fetal Neonatal Ed 2012;97:F110–5.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Kusuda, S., Fujimura, M., Uchiyama, A. et al. Trends in morbidity and mortality among very-low-birth-weight infants from 2003 to 2008 in Japan. Pediatr Res 72, 531–538 (2012). https://doi.org/10.1038/pr.2012.114
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.114
This article is cited by
-
Mortality and neurodevelopmental outcomes in very low birth weight infants with esophageal atresia
Pediatric Surgery International (2023)
-
Relationship of cerebral blood volume with arterial and venous flow velocities in extremely low-birth-weight infants
European Journal of Pediatrics (2023)
-
Sports participation and preterm birth: a nationwide birth cohort in Japan
Pediatric Research (2022)
-
Infant’s Behaviour Checklist for low birth weight infants and later neurodevelopmental outcome
Scientific Reports (2021)
-
Association of low birth weight with undernutrition in preschool-aged children in Malawi
Nutrition Journal (2019)