Abstract
Objective
It has been suggested that sustained-release valproate (VPA) formulations may be more effective and better tolerated than conventional VPA due to better compliance and lower fluctuations in VPA serum concentrations, but comparative trials with conventional VPA in children are scarce. This randomized and crossover trial compared the efficacy (complete control of seizures), the tolerability, and the patient (or parents) preference of conventional VPA twice daily (CVbid) with those of sustained-release chrono VPA twice daily (ChVbid), once daily in the morning (ChVom) or once daily in the evening (ChVoe) in monotherapy.
Methods
The study was carried out in 48 children (29 girls), aged 5–14 years, with newly diagnosed partial epilepsy (n=26), or idiopathic generalized epilepsy (n=22). The study duration was 16 months (four phases of 4 months each). VPA pharmacokinetics data were also compared in the different regimens. Mean VPA dosage was of approximately 870 mg/day (approximately 22 mg/kg/day) and mean VPA concentration was of approximately 89 mg/l at 12 h post-dose and of 54 mg/l at 24 h post-dose.
Results
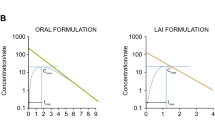
By intention in treatment there were no significant differences in efficacy (73%, 83%, 77% and 75%, respectively) or in adverse reaction frequency (56%, 58%, 67% and 46%, respectively). There were significant differences, however, in patient (or parents) preference, the order being ChVoe (31%) > ChVom (25%) > CVbid (17%) > ChVbid (8%). The mean VPA serum concentration fluctuation between 4 h and 0 h post-morning-dose was nonsignificantly lower after CVbid than after ChVbid. Fluctuation was significantly higher after ChVom than after CVbid or ChVbid. The mean VPA serum concentration difference between 12 h and 24 h post-dose was approximately 40 mg/l.
Conclusion
Although our results should be confirmed by a larger study, they suggest that the efficacy and tolerability of chrono valproate is similar to that of conventional valproate, and that the main advantage is the once-daily administration.


Similar content being viewed by others
References
Bialer M (1992) Pharmacokinetic evaluation of sustained release formulations of antiepileptic drugs. Clinical implications. Clin Pharmacokinet 22:11–21
Davis R, Peters DH, McTavish D (1994) Valproic acid: a reappraisal of its pharmacological properties and clinical efficacy in epilepsy. Drugs 47:332–372
Perucca E (2002) Pharmacological and therapeutic properties of valproate: a summary after 35 years of clinical experience. CNS Drugs 16:695–714
Covanis A, Jeavons PM (1980) Once-daily sodium valproate in the treatment of epilepsy. Dev Med Child Neurol 22:202–204
Covanis A, Gupta AK, Jeavons PM (1981) Monotherapy with once-daily sodium valproate (Epilim). In: Dam M, Gram L, Penry JK (eds) Advances in epileptology. XII Epilepsy International Symposium. Raven Press, New York, pp 527–532
Gjerloff I, Arentsen J, Alving J, Secher BG (1984) Monodose versus 3 daily doses of sodium valproate: a controlled trial. Acta Neurol Scand 69:120–124
Rowan AJ, Overweg J, Meijer JWA (1981) Monodose therapy with valproic acid: 24 hour telemetric EEG and serum level studies. In: Dam M, Gram L, Penry JK (eds) Advances in epileptology. XII Epilepsy International Symposium. Raven Press, New York, pp 533–539
Schmidt D (1977) Fluctuation of dipropyl acetate plasma levels with one and three daily doses. Pharm Weekbl (Sci) 112:285–287
Stefan H, Burr W, Fichsel H, Fröscher W, Penin H (1984) Intensive follow-up monitoring in patients with once daily administration of sodium valproate. Epilepsia 25:152–160
Barre J, Berger Y (1989) Pharmacokinetics of a newly developed sustained release form of sodium valproate. In: Chadwick D (ed) Fourth international symposium on sodium valproate and epilepsy. Royal Society of Medicine Services, London, pp 178–184
Roberts D, Easter D, O’Bryan-Tear G (1996) Epilim chrono: a multidose, crossover comparison of two formulations of valproate in healthy volunteers. Biopharm Drug Dispos 17:175–182
Mimaki T, Fukuyama Y, Otsuka S et al (1991) Clinical pharmacokinetics of NIK-240, a new slow release granule of sodium valproate, in epileptic children (in Japanese). Shonika Rinsho (Tokyo) 44:183–201
Imaizumi T, Izumi T, Fukuyama Y (1992) A comparative clinical and pharmacokinetic study of a new slow-release versus conventional preparations of valproic acid in children with intractable epilepsy. Brain Dev 14:304–308
Brouwer OF, Pieters MSM, Edelbroek PM et al (1992) Conventional and controlled release valproate in children with epilepsy: a cross-over study comparing plasma levels and cognitive performance. Epilepsy Res 13:245–253
Despland PA (1994) A retrospective study of 113 epileptic patients treated with sustained-release valproate. Epilepsia 35(Suppl 5):99–100
Wieser HG (1991) Comparison of valproate concentrations in human plasma, CSF and brain tissue after administration of different formulations of valproate or valpromide. Epilepsy Res 9:154–159
Ieiri I, Morioka T, Ichimiya T et al (1995) Pharmacokinetic study of valproic acid sustained-release preparation in patients undergoing brain surgery. Ther Drug Monit 17:6–11
Doughty J, Baker GA, Jacoby A, Lavaud V (2003) Compliance and satisfaction with switching from an immediate-release to sustained-release formulation of valproate in people with epilepsy. Epilepsy Behav 4:710–716
Mimaki T, Fukuyama Y, Abe T et al (1990) Clinical study of NIK-240, a new slow release granule of sodium valproate in epileptic children. Cross-over comparison to Depakine granule (in Japanese). Shonika Rinsho (Tokyo) 43:2970–2976
Rinnerthaler M, Luef G, Mueller J et al (2005) Computerized tremor analysis of valproate-induced tremor: a comparative study of controlled-release versus conventional valproate. Epilepsia 46:320–323
Thibault M, Blume WT, Saint-Hilaire JM, Zakhari R, Sommerville KW (2005) Divalproex extended-release versus the original divalproex tablet: results of a randomized, crossover study of well-controlled epileptic patients with primary generalized seizures. Epilepsy Res 50:243–249
Cenraud B, Guyot M, Levy RH, Brachet-Liermain A, Morselli PL, Loiseau P (1981) Effect of dosage regimen on valproic acid plasma levels. In: Dam M, Gram L, Penry JK (eds) Advances in epileptology: XIIth epilepsy international symposium. Raven Press, New York, pp 549–553
Chadwick DW (1985) Concentration-effect relationships of valproic acid. Clin Pharmacokinet 10:155–163
Glauser TA, Pippenger CE (2000) Controversies in blood-level monitoring: reexamining its role in the treatment of epilepsy. Epilepsia 41(Suppl 8):6–15
Vajda F, Morris P, Drummer O, Bladin P (1976) In: Legg NJ (ed) Clinical and pharmacological aspects of sodium valproate in the treatment of epilepsy. Tunbridge Wells, Kent, pp 91–100
Gram L, Flachs H, Wurtz-Jorgensen A, Parnas J, Andersen B (1979) Sodium valproate, serum level and clinical effect in epilepsy: a controlled study. Epilepsia 20:303–312
Beydoun A, Sackellares JC, Shu V (1997) Safety and efficacy of divalproex sodium monotherapy in partial epilepsy: a double-blind, concentration-response design clinical trial. Neurology 48:182–188
Goggin T, Casey C, Callaghan N (1986) Serum levels of sodium valproate, phenytoin and carbamazepine and seizure control in epilepsy. Irish Med J 79:150–156
Turnbull DM, Rawlins MD, Weightman D, Chadwick DW (1983) Plasma concentrations of sodium valproate: their clinical value. Ann Neurol 14:38–42
Acknowledgements
The study was performed with informed consent and following all the guidelines for experimental investigation with human subjects required by the Drug Spanish Agency, as well as the Helsinki Declaration of 1975 as revised in 1996. The protocol of this randomized, comparative and crossover phase IV clinical trial was approved by the Ethics Committee of the Marques de Valdecilla University Hospital and the Drug Spanish Agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Herranz, J.L., Arteaga, R., Adín, J. et al. Conventional and sustained-release valproate in children with newly diagnosed epilepsy: a randomized and crossover study comparing clinical effects, patient preference and pharmacokinetics. Eur J Clin Pharmacol 62, 805–815 (2006). https://doi.org/10.1007/s00228-006-0175-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-006-0175-2