Abstract
Objective:
We hypothesized that the implementation of a neonatal palliative care initiative will result in improved markers of end-of-life care.
Study design:
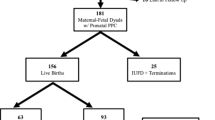
A retrospective and prospective chart review of neonatal intensive care unit deaths was performed for 24 months before, 16 months during and 24 months after the implementation of palliative care provider education and practice guidelines (n=106). Ancillary care, redirection of care, palliative medication usage and outcome meetings in the last 48 h of life and basic demographic data were compared between epochs. Parametric and nonparametric analysis was performed.
Result:
There was an increase in redirection of care and palliative medication usage and a decrease in variability of use of end-of-life interventions (P=0.012, 0.022 and <0.001).
Conclusion:
The implementation of a neonatal palliative care initiative was associated with increases in palliative interventions for neonates in their final 48 h of life, suggesting that such an initiative may enhance end-of-life care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Murphy SL, Xu J, Kochanek KD . Deaths: final data for 2010. Natl Vital Stat Rep 2013; 61 (4): 1–117.
Brandon D, Docherty SL, Thorpe J . Infant and child deaths in acute care settings: implications for palliative care. J Palliat Med 2007; 10 (4): 910–918.
Cortezzo DE, Sanders MR, Brownell E, Moss K . Neonatologists' perspectives of palliative and end-of-life care in neonatal intensive care units. J Perinatol 2013; 33 (9): 731–735.
Feudtner C, Womer J, Augustin R, Remke S, Wolfe J, Friebert S et al. Pediatric palliative care programs in children's hospitals: a cross-sectional national survey. Pediatrics 2013; 132 (6): 1063–1070.
Keele L, Keenan HT, Sheetz J, Bratton SL . Differences in characteristics of dying children who receive and do not receive palliative care. Pediatrics 2013; 132 (1): 72–78.
Martin M . Missed opportunities: a case study of barriers to the delivery of palliative care on neonatal intensive care units. Int J Palliat Nurs 2013; 19 (5): 251–256.
El Sayed MF, Chan M, McAllister M, Hellmann J . End-of-life care in Toronto neonatal intensive care units: challenges for physician trainees. Arch Dis Child Fetal Neonatal Ed 2013; 98 (6): F528–F533.
Boss RD, Hutton N, Donohue PK, Arnold RM . Neonatologist training to guide family decision making for critically ill infants. Arch Pediatr Adolesc Med 2009; 163 (9): 783–788.
Wool C . Clinician confidence and comfort in providing perinatal palliative care. J Obstet Gynecol Neonatal Nurs 2013; 42 (1): 48–58.
Carter BS, Bhatia J . Comfort/palliative care guidelines for neonatal practice: development and implementation in an academic medical center. J Perinatol 2001; 21 (5): 279–283.
Catlin A, Carter BS . Creation of a neonatal end-of-life palliative-care protocol. J Clin Ethics 2001; 12 (3): 316–318.
Pierucci RL, Kirby RS, Leuthner SR . End-of-life care for neonates and infants: the experience and effects of a palliative care consultation service. Pediatrics 2001; 108 (3): 653–660.
Gale G, Brooks A . Implementing a palliative care program in a newborn intensive care unit. Adv Neonatal Care 2006; 6 (1): 37–53.
American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics 2000; 106 (2 Pt 1): 351–357.
Hoyert DL, Heron MP, Murphy SL, Kung HC . Deaths: final data for 2003. Natl Vital Stat Rep 2006; 54 (13): 1–120.
Feudtner C, Hexem KR, Shabbout M, Feinstein JA, Sochalski J, Silber JH . Prediction of pediatric death in the year after hospitalization: a population-level retrospective cohort study. J Palliat Med 2009; 12 (2): 160–169.
Williams-Reade J, Lamson AL, Knight SM, White MB, Ballard SM, Desai PP . The clinical, operational, and financial worlds of neonatal palliative care: a focused ethnography. Palliat Support Care 2013 (e-pub ahead of print).
Kiman R, Doumic L . Perinatal palliative care: a developing specialty. Int J Palliat Nurs 2014; 20 (3): 143–148.
Lago P, Boccuzzo G, Garetti E, Pirelli A, Pieragostini L, Merazzi D et al. Pain management during invasive procedures at Italian NICUs: has anything changed in the last five years? J Matern Fetal Neonatal Med 2013; 26 (3): 303–305.
Byrd PJ, Gonzales I, Parsons V . Exploring barriers to pain management in newborn intensive care units: a pilot survey of NICU nurses. Adv Neonatal Care 2009; 9 (6): 299–306.
Matthews AL, O'Conner-Von S . Administration of comfort medication at end of life in neonates: effects of weight. Neonatal Netw 2008; 27 (4): 223–227.
Janvier A, Meadow W, Leuthner SR, Andrews B, Lagatta J, Bos A et al. Whom are we comforting? An analysis of comfort medications delivered to dying neonates. J Pediatr 2011; 159 (2): 206–210.
Wright V, Prasun MA, Hilgenberg C . Why is end-of-life care delivery sporadic? A quantitative look at the barriers to and facilitators of providing end-of-life care in the neonatal intensive care unit. Adv Neonatal Care 2011; 11 (1): 29–36.
Randolph AG, Zollo MB, Egger MJ, Guyatt GH, Nelson RM, Stidham GL . Variability in physician opinion on limiting pediatric life support. Pediatrics 1999; 103 (4): e46.
Feudtner C, Kang TI, Hexem KR, Friedrichsdorf SJ, Osenga K, Siden H et al. Pediatric palliative care patients: a prospective multicenter cohort study. Pediatrics 2011; 127 (6): 1094–1101.
Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK . Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. Pediatrics 2008; 122 (3): 583–589.
Fontana MS, Farrell C, Gauvin F, Lacroix J, Janvier A . Modes of death in pediatrics: differences in the ethical approach in neonatal and pediatric patients. J Pediatr 2013; 162 (6): 1107–1111.
Janvier A, Barrington K, Farlow B . Communication with parents concerning withholding or withdrawing of life-sustaining interventions in neonatology. Semin Perinatol 2014; 38 (1): 38–46.
Meyer EC, Ritholz MD, Burns JP, Truog RD . Improving the quality of end-of-life care in the pediatric intensive care unit: parents' priorities and recommendations. Pediatrics 2006; 117 (3): 649–657.
Dussel V, Kreicbergs U, Hilden JM, Watterson J, Moore C, Turner BG et al. Looking beyond where children die: determinants and effects of planning a child's location of death. J Pain Symptom Manage 2009; 37 (1): 33–43.
Carter BS, Guthrie SO . Utility of morbidity and mortality conference in end-of-life education in the neonatal intensive care unit. J Palliat Med 2007; 10 (2): 375–380.
Carter BS, Howenstein M, Gilmer MJ, Throop P, France D, Whitlock JA . Circumstances surrounding the deaths of hospitalized children: opportunities for pediatric palliative care. Pediatrics 2004; 114 (3): e361–e366.
Moura H, Costa V, Rodrigues M, Almeida F, Maia T, Guimaraes H . End of life in the neonatal intensive care unit. Clinics (Sao Paulo) 2011; 66 (9): 1569–1572.
Carter BS, Hubble C, Weise KL . Palliative medicine in neonatal and pediatric intensive care. Child Adolesc Psychiatr Clin N Am 2006; 15 (3): 759–777.
Ewing AE, Carter BS . Once again, Vanderbilt NICU in Nashville leads the way in nurses' emotional support. Pediatr Nurs 2004; 30 (6): 471–472.
Janvier A, Nadeau S, Deschenes M, Couture E, Barrington KJ . Moral distress in the neonatal intensive care unit: caregiver's experience. J Perinatol 2007; 27 (4): 203–208.
Cavaliere TA, Daly B, Dowling D, Montgomery K . Moral distress in neonatal intensive care unit RNs. Adv Neonatal Care 2010; 10 (3): 145–156.
Okah FA, Wolff DM, Boos VD, Haney BM, Oshodi AA . Perceptions of a strategy to prevent and relieve care provider distress in the neonatal intensive care unit. Am J Perinatol 2012; 29 (9): 687–692.
Rogers S, Babgi A, Gomez C . Educational interventions in end-of-life care: part I: an educational intervention responding to the moral distress of NICU nurses provided by an ethics consultation team. Adv Neonatal Care 2008; 8 (1): 56–65.
Acknowledgements
We would like to thank the Women and Infants Hospital NICU Palliative Care working group for their critical input.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Samsel, C., Lechner, B. End-of-life care in a regional level IV neonatal intensive care unit after implementation of a palliative care initiative. J Perinatol 35, 223–228 (2015). https://doi.org/10.1038/jp.2014.189
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.189
This article is cited by
-
Infant mode of death in the neonatal intensive care unit: A systematic scoping review
Journal of Perinatology (2022)
-
Neonatal palliative care: perception differences between providers
Journal of Perinatology (2020)
-
Parental assessment of comfort in newborns affected by life-limiting conditions treated by a standardized neonatal comfort care program
Journal of Perinatology (2018)
-
Survival and healthcare utilization of infants diagnosed with lethal congenital malformations
Journal of Perinatology (2018)
-
Introduction of triggers for palliative care consultation improves utilization and satisfaction within a level four NICU
Journal of Perinatology (2018)