Abstract
BACKGROUND:
Inhaled nitric oxide (iNO) is an effective adjunct in the treatment of infants with respiratory failure. Although there are clear benefits to this therapy, potential toxicity could result from reactive nitrosylated species.
OBJECTIVE:
To evaluate whether iNO therapy is associated with increased serum markers of oxidative stress.
DESIGN/METHOD:
Multiple markers were prospectively evaluated in the serum of term infants with severe respiratory failure treated with iNO for 1 to 72 hours. These were compared to those of patients exposed to greater than 80% oxygen for more than 6 hours and room air controls.
RESULTS:
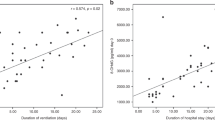
After 24 hours of exposure, the iNO-treated infants had increased serum lipid hydroperoxides (LPO), protein carbonyls and nitrotyrosine residues as well as increased serum total glutathione (GSH) content. The increase in LPO peaked at 24 hours and correlated with the cumulative dose of iNO whereas other markers did not. The presence of chronic lung disease (CLD) did not correlate with serum markers of oxidative injury.
CONCLUSIONS:
In term infants with respiratory failure, prolonged iNO exposure is associated with a transient increase in markers of oxidative stress, but this finding does not appear to predict the development of CLD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Davis JM, Spitzer AR, Cox C, Fox WW . Predicting survival in infants with persistent pulmonary hypertension of the newborn. Pediatr Pulmonol 1988;5:6–9.
Hageman JR, Dusik J, Keuler H, Bregman J, Gardner TH . Outcome of persistent pulmonary hypertension in relation to severity of presentation. Am J Dis Child 1988;142:293–296.
Gersony WM . Neonatal pulmonary hypertension: pathophysiology, classification, and etiology. Clin Perinatol 1984;11:517–524.
Roberts JD, Fineman JR, Morin FC, et al. Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. N Engl J Med 1997;336:605–610.
The Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med 1997;336:597–604.
Clark RH, Kueser TJ, Walker MW, et al. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Research Group. N Engl J Med 2000;342:469–474.
Austin AT . The chemistry of the higher oxides of nitrogen as related to the manufacture, storage and administration of nitrous oxide. Br J Anaesth 1967;39:345–350.
Foubert L, Fleming B, Latimer R, et al. Safety guidelines for use of nitric oxide [letter] [see comments]. Lancet 1992;339:1615–1616.
Robbins CG, Horowitz S, Merritt TA, et al. Recombinant human superoxide dismutase reduces lung injury caused by inhaled nitric oxide and hyperoxia. Am J Physiol 1997;272:L903–L907.
Gutierrez HH, Nieves B, Chumley P, Rivera A, Freeman BA . Nitric oxide regulation of superoxide-dependent lung injury: oxidant-protective actions of endogenously produced and exogenously administered nitric oxide. Free Radic Biol Med 1996;21:43–52.
Storme L, Zerimech F, Riou Y, et al. Inhaled nitric oxide neither alters oxidative stress parameters nor induces lung inflammation in premature lambs with moderate hyaline membrane disease. Biol. Neonate 1998;73:172–181.
Lorch SA, Banks BA, Christie J, et al. Plasma 3-nitrotyrosine and outcome in neonates with severe bronchopulmonary dysplasia after inhaled nitric oxide. Free Radic Biol Med 2003;34:1146–1152.
Haddad IY, Pataki G, Hu P, et al. Quantitation of nitrotyrosine levels in lung sections of patients and animals with acute lung injury. J Clin Invest 1994;94:2407–2413.
Ohishi N, Ohkawa H, Miike A, Tatana T, Yagi K . A new assay method for lipid peroxides using a methylene blue derivative. Biochem Int 1985;10:205–211.
Beckman JS, Beckman TW, Chen J, Marshall PA, Freeman BA . Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci USA 1990;87:1620–1624.
Halliwell B . Oxidants and human disease: some new concepts. FASEB J 1987;1:358–364.
Kinsella JP, Parker TA, Galan H, Sheridan BC, Halbower AC, Abman SH . Effects of inhaled nitric oxide on pulmonary edema and lung neutrophil accumulation in severe experimental hyaline membrane disease. Pediatr Res 1997;41:457–463.
Ben Baouali A, Aube H, Maupoil V, Blettery B, Rochette L . Plasma lipid peroxidation in critically ill patients: importance of mechanical ventilation. Free Radic Biol Med 1994;16:223–227.
Kokk T, Talvik R, Zilmer M, Kutt E, Talvik T . Markers of oxidative stress before and after exchange transfusion for neonatal sepsis. Acta Paediatr 1996;85:1244–1246.
Dominguez C, Ruiz E, Gussinye M, Carrascosa, A . Oxidative stress at onset and in early stages of type 1 diabetes in children and adolescents. Diabetes Care 1998;21:1736–1742.
Inouye M, Hashimoto H, Mio T, Sumino K . Levels of lipid peroxidation product and glycated hemoglobin A1c in the erythrocytes of diabetic patients. Clin Chim Acta 1998;276:163–172.
Jornot L, Junod AF . Variable glutathione levels and expression of antioxidant enzymes in human endothelial cells. Am J Physiol 1993;264:L482–L489.
Kennedy KA, Lane NL . Effect of in vivo hyperoxia on the glutathione system in neonatal rat lung. Exp Lung Res 1994;20:73–83.
Ho YS, Dey MS, Crapo JD . Antioxidant enzyme expression in rat lungs during hyperoxia. Am J Physiol 1996;270:L810–L818.
Silvers KM, Gibson AT, Russell JM, Powers HJ . Antioxidant activity, packed cell transfusions, and outcome in premature infants. Arch Dis Child Fetal Neonatal Ed 1998;78:F214–F219.
Gladstone Jr IM, Levine RL . Oxidation of proteins in neonatal lungs. Pediatrics 1994;93:764–768.
Varsila E, Pitkanen O, Hallman M, Andersson S . Immaturity-dependent free radical activity in premature infants. Pediatr Res 1994;36:55–59.
Winterbourn CC, Chan T, Buss IH, Inder TE, Mogridge N, Darlow BA . Protein carbonyls and lipid peroxidation products as oxidation markers in preterm infant plasma: associations with chronic lung disease and retinopathy and effects of selenium supplementation. Pediatr Res 2000;48:84–90.
Banks BA, Ischiropoulos H, McClelland M, Ballard PL, Ballard RA . Plasma 3-nitrotyrosine is elevated in premature infants who develop bronchopulmonary dysplasia. Pediatrics 1998;101:870–874.
Acknowledgements
The authors thank Patricia Hartsell, RN and Dorothy Inguilo, RN for their invaluable assistance in collecting samples. This work was funded in part by the Child Health Research Fund of Lucile Packard Children's Hospital at Stanford University, and in part by Grant 5 M01-RR00070 from the National Center for Research Resources, National Institutes of Health.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Van Meurs, K., Cohen, T., Yang, G. et al. Inhaled NO and Markers of Oxidant Injury in Infants with Respiratory Failure. J Perinatol 25, 463–469 (2005). https://doi.org/10.1038/sj.jp.7211327
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211327